In Light at the End of the Tunnel (read now if you haven’t yet), I described the challenge my doctor faced as I lay on a continuous x-ray machine in a space-age operating room at the Brigham on Friday, June 15. A cholesterol plaque had ruptured in my right coronary artery five days earlier at the finish line of the Light at the End of the Tunnel Marathon. The resulting clotting triggered by the rupture had resulted in an undetected myocardial infarction (a heart attack).

My interventional cardiologist, Dr. Jane Leopold, had run a razor-thin catheter through my wrist into the right chamber of my heart and injected a pulse of X-ray imaging dye. This dye should have flowed down into my right coronary artery (RCA) up to the point of the blockage, but the clogged RCA was invisible. My EKG had correctly pointed to it being the problem, and sure enough, it was fully obstructed by a blood clot flush right up to its entrance. The lack of penetration hid the path to clear the 5-day old clot that was starving a portion of my heart of oxygen.
Faced with this problem, Dr. Leopold could have called it a night and left things as they were. I was mostly stable, with the effects of my 2nd, milder, heart attack that morning having subsided. Many people today are unknowingly walking around with reduced function, having survived undetected heart attacks. At some point, it is too late to clear a dead artery feeding dead heart muscle. Alternatively, she could have rolled me over to surgery to have a heart surgeon cut through my sternum for a single bypass with its associated risks and extended recovery. Neither was a good option for me.
Instead, she persisted.
She sent a 2nd catheter up my femoral vein from my hip into the left chamber of the heart. The X-ray dye injected there showed the Left Coronary Artery and its”widow-maker” left-anterior descending artery (LAD), open and in good shape.
But there was something more —at the end of the video — flow across the heart from the left artery entering my right artery.
Collateral arteries are not well-understood and still the subject of active research. About 2% of us have them from birth. A subset of the population can also develop them through regular exercise as a form of do-it-yourself bypass surgery. As cholesterol builds up, the pressure downstream of the flow restriction drops. A trace amount of blood flows through tiny capillaries toward it from higher pressure areas of the heart due to this pressure differential.
The walls of the capillaries are programmed to sense the shearing forces of the blood rushing past and trigger the capillary walls to grow to be a functioning artery, like water in a winding river finding the path of least resistance and eroding new pathways. When a cholesterol rupture event suddenly blocks the narrowing artery, the collaterals slowly expand to deliver flow to the starved area.
As luck would have it, I have a robust set of collateral arteries, and they were a double blessing that Friday evening.
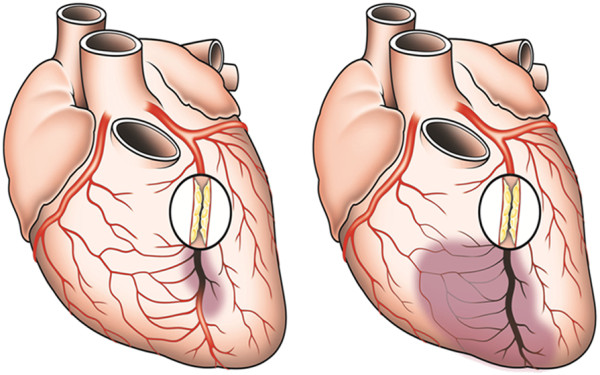
First, the collateral arteries had provided enough oxygen to prevent significant damage to my heart muscle. Often patients with a 100% clogged RCA will lose vital heart function. I met such a person in subsequent cardiac rehab. Second, they were now delivering the x-ray dye to the backside of my blockage and illuminating the obstruction.
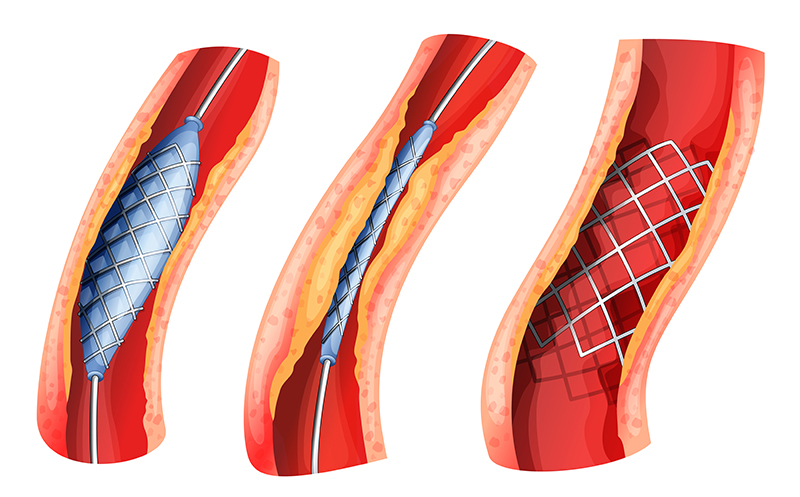
With the artery located, Dr. Leopold inserted yet another catheter up a third blood vessel, this time, through my femoral artery. She navigated to the entrance of the RCA and used dye pulses from the two catheters to guide a careful extraction of the hardened chunks of the 5-day old clot. If she inadvertently released a clot fragment into the right chamber, it would be pumped to my lungs, and trigger a dangerous pulmonary embolism. I imagine this was like a game of Operation, but done remotely by controlling a few feet of nano-wire, rather than a set of tweezers.
Once she had cleared the artery and ballooned it open, she stabilized it with two stents and restored normal flow.
My procedure played out over three hours on the x-ray table. I had not thought to take off my Garmin, and thus my heart rate was recorded for posterity throughout the procedure. I know some of you are saying, “Yeah, right, you wanted the data to analyze…”
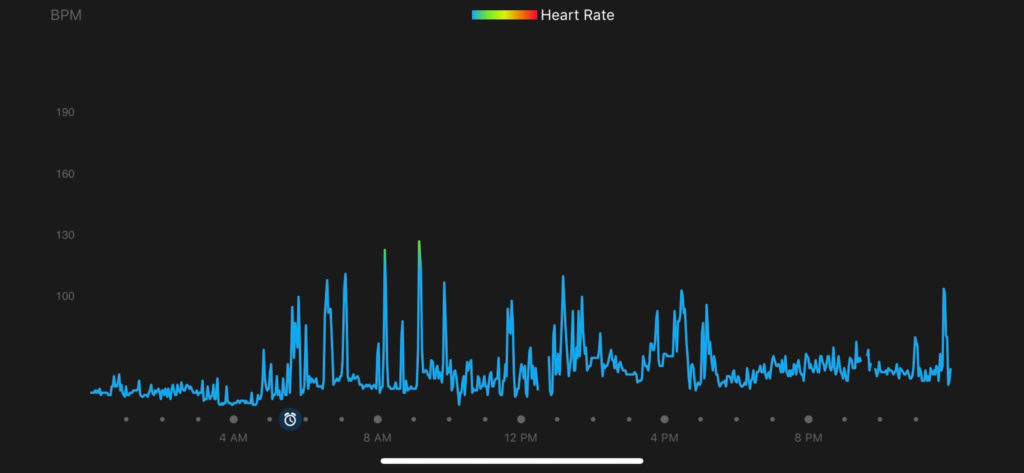
It didn’t miss a beat or show any signs of stress. While I was conscious through most of the procedure, I was fed fentanyl and an amnesia medication that inhibits short-term memory formation. Mostly what I remember was being told not to move my right arm and, with increasing sternness, to stop asking questions so that the team could focus. Of course, I forgot these instructions repeatedly due to the short term amnesia drug.
I rolled into the recovery room at 9 PM. The challenge now was to keep my artery punctures sealed despite a body pumped with anticoagulants. I lay flat on my back for the night, which was not ideal — They had infused me with several liters of saline and diuretic x-ray dye. The next day I had a normal echocardiogram and effortlessly walked two miles in the hallway.
I dedicated my Sunday Strava entry to Brooks runner Gabe Grunewald, who suffered from a rare disease that repeatedly triggered cancers in her body. My daughter had the honor of interviewing her at Brooks in 2017. Gabe had passed away that Tuesday, but not before making it clear to the world she was going to decide when to go (#NotToday). I had #BraveLikeGabe in my thoughts the whole week, from the marathon to the “indigestion,” to that first return to extended walking. And in how to live since then.
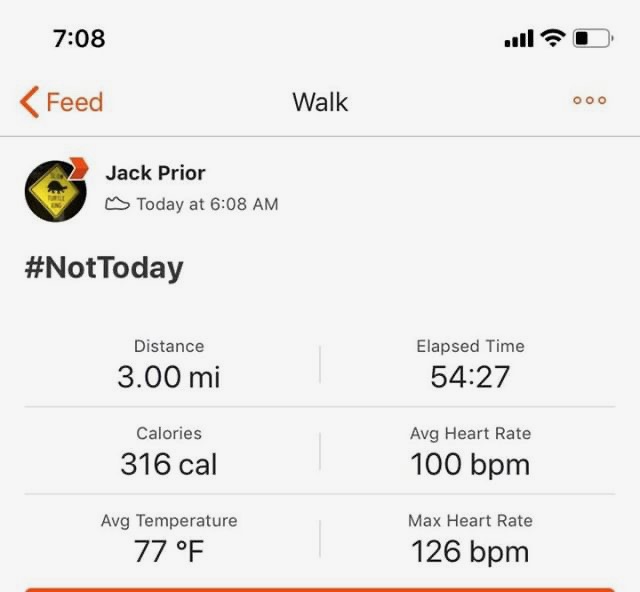
One could argue the strain of the marathon effort and the final sprint triggering my cholesterol plaque rupture at the finish line. The truth is it was going to happen sooner or later. Had it happened without the collaterals developed through training for the marathon, the outcome would have been significantly worse. Miraculously, a stress test two weeks later showed no functional damage or reduction in my running fitness. I was cleared to return to running and finished a tempo-effort 5K just 25 days out of the hospital.
I had been thrilled to just be able to jog slowly, but with an improved diet and 10% weight loss over the subsequent months, I am now 10% faster than before the event — so no need for any sympathies! My 3mile PR improved from 22 to 20 min and my half marathon improved from 1:46 to 1:36 — basically all due to the heart being same and weight going down.
So on this Thanksgiving Day, I am beyond thankful.
Thankful to Dr. Leopold for her skill and persistence, and to her team for being at the ready at the Brigham to treat me for three hours late on Friday evening.
Thankful to the scientists and engineers who developed the advanced technologies and numerous medications brought to bear to make the procedure and subsequent therapy a success.
Thankful to my family, friends, and support team who encouraged and supported my journey back to fitness before this event, and my return to health after.
You saved my quality of life, and likely my life itself.
Read Next: Please take your ticket.

[Note: I will be running the 125th Boston Marathon to raise scholarship funds for Newton Rotary. This blog will share the journey to the starting line past and future. In particular, I’ll be sharing what I’ve learned about cardiovascular health in the hope of helping others in prevention as we as detection. Subscribe to follow along. Support Rotary scholarships if you can.]



Thank you for taking the time to bring awareness, share your story and for being so wonderful always. Love the Priors!!!!
Jack. This is quite a story. I am so glad you are recovering. Thanks for sharing.
Were there any prescription guidance to lower cholesterol as well as long term changes in diet after this event? Any advice for preventative measures?
Hi Ziran — Answering those questions will be the topic of a future post. Recent clinical studies show there is no point of diminishing returns when reducing bad cholesterol. People with marginal cholesterol numbers really should consider statins. The bad/good ratio is much more important than I realized years ago. Basic diet advice is to follow the Mediterranean diet along with Micheal Polin’s advice – “eat food, mostly plants, not too much”. Avoid processed foods, sugar, and inflammation.
Great story!